Cancer Deaths Disproportionately Affecting Deprived Areas in Northern Ireland
A recent report from Cancer Research UK has shed light on the stark reality of cancer deaths in Northern Ireland, revealing that individuals residing in the most deprived areas face a 45% higher risk of succumbing to this devastating disease compared to those in the least deprived regions. This alarming statistic underscores the urgent need for targeted interventions to address the glaring health inequalities prevalent in the region, where approximately 630 additional lives are lost to cancer each year due to socioeconomic disparities.
The Impact of Socioeconomic Deprivation on Cancer Mortality
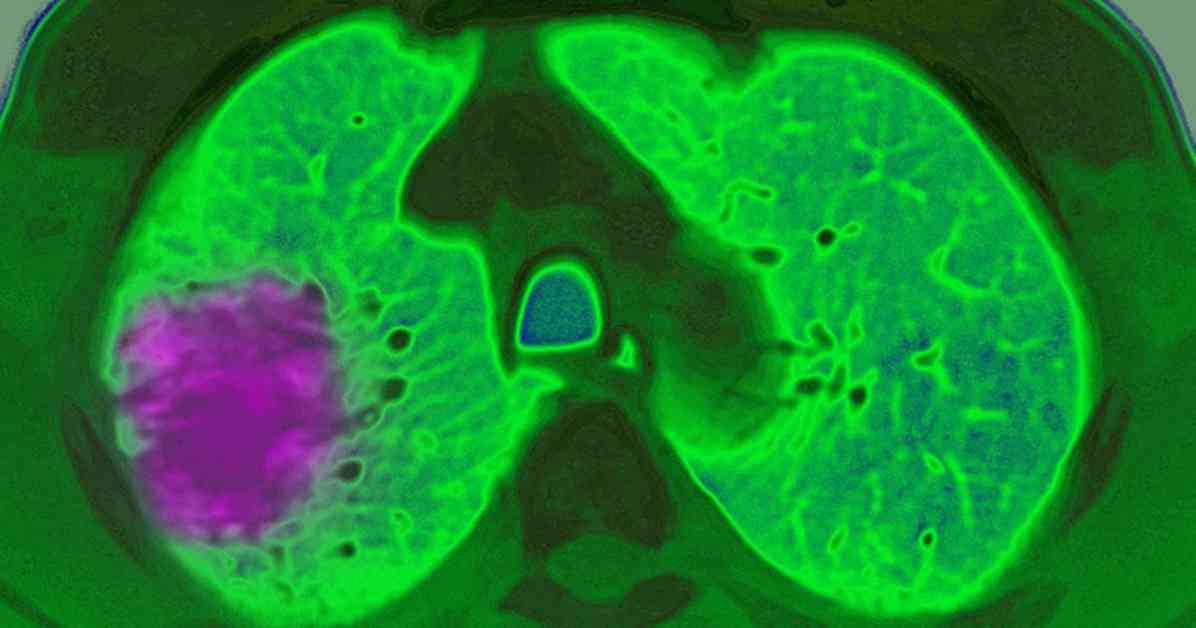
The report, titled “Cancer in the UK 2025: Socioeconomic Deprivation,” paints a concerning picture of the impact of socioeconomic factors on cancer mortality rates in Northern Ireland. It highlights the disproportionate burden borne by individuals in deprived areas, with nearly two additional deaths occurring daily – equating to three out of every 20 cancer-related deaths in the region. Lung cancer emerges as a significant contributor to this disparity, responsible for approximately 60% of the excess mortality observed in deprived areas.
One of the key findings of the report is the revelation that almost 10% of all cancer diagnoses in Northern Ireland can be attributed to deprivation, with preventable risk factors such as smoking playing a significant role in driving these alarming figures. Smoking, the leading cause of cancer in the country, is particularly prevalent in deprived communities, where rates are more than triple those in affluent areas.
The Call for Urgent Action and a Lung Cancer Screening Programme
In response to these troubling revelations, Cancer Research UK is urging policymakers and healthcare authorities in Northern Ireland to take swift action to address these glaring health inequities. One crucial intervention recommended by the organization is the implementation of a lung cancer screening programme tailored to individuals at high risk of developing the disease.
The UK National Screening Committee has endorsed the introduction of lung cancer screening for individuals aged between 55 and 74 who have a history of smoking or are current smokers. While England has already initiated a targeted screening programme, Northern Ireland, along with Scotland and Wales, has yet to implement this life-saving intervention. The potential benefits of such a programme are significant, with projections indicating that early detection through screening could lead to the diagnosis of 140 additional cases annually at stages 1 and 2, when treatment is most effective.
Expert Insights and Advocacy for Change
Liz Morrison, Cancer Research UK’s public affairs manager in Northern Ireland, emphasizes the critical role of lung cancer screening in reducing cancer-related mortality. She underscores the importance of early detection in improving treatment outcomes and stresses the need for comprehensive, system-wide reforms to address the pressing healthcare challenges faced by the region.
Recent legislative developments, such as the Age of Sale legislation aimed at curbing tobacco sales to minors, mark positive steps towards combating the root causes of cancer in Northern Ireland. However, more concerted efforts are needed to address the structural inequalities that perpetuate disparities in cancer outcomes, as highlighted by SDLP Opposition Health Spokesperson Colin McGrath.
McGrath’s call for urgent action and equitable access to healthcare resonates with the Department of Health’s commitment to addressing health inequalities through initiatives like the Live Better programme. While progress is being made in streamlining cancer diagnosis and treatment pathways, substantial investment and collaboration across multiple sectors will be crucial in ensuring equitable access to quality care for all residents of Northern Ireland.
As the region grapples with the complex challenges posed by socioeconomic deprivation and its impact on cancer outcomes, the need for coordinated, evidence-based interventions has never been more pressing. By prioritizing early detection, preventive strategies, and equitable access to healthcare services, policymakers and healthcare providers can work towards reducing the burden of cancer in Northern Ireland and ensuring that all individuals have the opportunity to live healthier, longer lives.